Shoulder Replacement
shoulder replacement is a highly beneficial surgical procedure intended to reduce pain and restore mobility in patients with end-stage shoulder arthritis and, occasionally, after certain severe shoulder fractures. One year after surgery, 95% of patients enjoy pain-free function, enabling them to exercise the shoulder area sufficiently to promote restoration of strength and motion. Most shoulder replacement patients successfully return to the activities they enjoy, making the procedure a highly valued choice for a wide variety of people who have shoulder pain due to cartilage loss.
Since its introduction in the United States in the 1950s, the procedure has been refined by combinations of improvement in surgical, anesthesia, and rehabilitation techniques. HSS surgeons have been instrumental in developing new materials, designs and techniques.
What is shoulder replacement surgery?

Total shoulder replacement, also known as total shoulder arthroplasty, is a tremendously successful procedure for treating the severe pain and stiffness that often result at the end-stage of various forms of arthritis or degenerative joint disease of the shoulder joint. The primary benefit of shoulder replacement surgery is pain relief. Additional benefits include the restoration of motion, strength and function to help patients return to an activity level as near to normal as possible. Many patients return to the sports they love like tennis, golf, and swimming, while also pursuing personal health initiatives such as individual training, yoga and pilates.
What causes the conditions treated by joint replacement surgery?
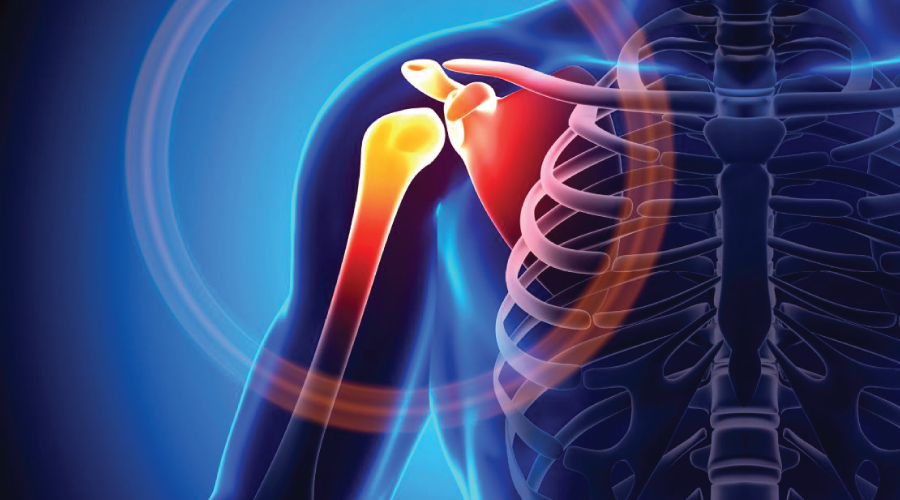
Painful shoulder arthritis refers to the disappearing of the normally smooth cartilage surfaces of the shoulder that permits the ball and socket of the joint to smoothly glide against one another. This disappearance of cartilage covering results in a “bone on bone” joint, which can be quite painful. Surgically implanted new surfaces provide a restoration of comfort..
Diagnosis of shoulder replacement surgery candidates
The most common indication that a person should get a shoulder replacement is shoulder pain due to arthritis that cannot be controlled with nonsurgical treatments. Such pain is usually accompanied by a progressive stiffness and loss of motion, in which patients often experience a grinding or grating sensation within the shoulder joint. These symptoms and sensations indicate that bones of the ball and socket are rubbing against one another because the cartilage that should lie between them has worn away.
A series of standard X-rays are taken to determine the condition of the shoulder joint (See Figure 1). A CT scan, which is a specialized X-ray, and magnetic resonance imaging (MRI), may also be necessary to evaluate a patient’s bone quality as well as the condition of important surrounding tissues, such as the rotator cuff tendon.
If nerve damage is suspected based on the doctor’s discussions with the patient, an EMG test or nerve conduction study may be ordered to evaluate the nerves that feed the important muscles of the shoulder.
Some patients experiencing early osteoarthritis may consider more conservative management of their condition to determine whether a shoulder replacement is necessary or may be delayed. Such measures include:
Who should not get a shoulder replacement?
Certain patients are contraindicated (not good candidates) for shoulder replacement. These include those:
Alternative surgeries for certain patients
For many shoulder conditions involving the surrounding ligaments, muscles and tendons – such as a rotator cuff injury or a torn shoulder labrum – a shoulder arthroscopy procedure is frequently recommended. Arthroscopy is among the most common type of shoulder surgeries, and is attractive to many patients because it is minimally invasive. However, arthroscopic surgery primarily treats conditions that cause arthritis. For arthritis patients, it is generally useful only before the arthritis of the joint has truly become “bone on bone.”
Overview of the procedure, anesthesia and types of implants
In shoulder replacement surgery, the damaged humeral head (or joint “ball”) is replaced with a metal ball, and a smooth plastic surface replaces the glenoid (or joint “socket”) – see Figure 2. Metal-on-plastic surfaces (rather than-metal-on metal) are the hallmark of virtually all shoulder replacement implant systems. Partial shoulder replacement (or hemireplacement) may also be recommended for patients with certain severe shoulder fractures of the humeral head. This technique requires the replacement of the ball component only.
The design of the reverse shoulder attaches a ball implant on the patients own natural socket, and a new plastic socket implant is placed on the humerus bone. The reverse design (where the positions of the ball and socket are switched) has more stability and does not need the tendons to hold it in place. It also is moved by the deltoid muscle, not the rotator cuff tendon, so it is an ideal choice when the damaged shoulder needs new surfaces, but does not have healthy enough soft tissues for stabilization and movement.
The design rationale for the reverse shoulder replacement is based on the fact that since in nature the shoulder ball “rests against” the socket (rather than being deeply contained within the socket) it relies on the tendons surrounding the ball socket to both hold it in place and to move it. In some types of arthritis, these tendons are severely damaged, torn, or non functioning. Because of this, an anatomic shoulder has no soft tissue to hold it in place and or to move it.
Anesthesia
For total shoulder replacement, regional anesthesia with interscalene block or general anesthesia may be used (or both, in many cases). During the operation, the patient will be sedated and unconscious, positioned in a sitting-up, position.
Surgical steps of an anatomic shoulder replacement
The surgery is composed of the following six basic steps:
Types of implant materials
In anatomic shoulder replacements
Many different types of implants are used in anatomic shoulder replacements. They all, however, share the same basic components: a metal ball that rests against a plastic (polyethylene) socket. The goal of shoulder replacement is to remove the patient’s arthritic humeral head, replace it with the metal “ball” component attached to a stem that extends down inside the patient’s humerus (upper arm bone), and then place a plastic socket over the surface of the patient’s own glenoid (See Figure 2). The polyethylene socket is often cemented to the bone surrounding it, at least in part, so that fixation to the bone is immediate. The prosthetic ball has a stem that is usually placed inside the humerus without the need for cement. In most cases, new prostheses feature stems that actually promote natural bone growth into the material.
In anatomic shoulder replacements
In a reverse shoulder , the components, while still metal and plastic, are reversed: The metal ball is attached to the patient’s existing socket, and a new plastic socket is attached to the patient’s upper humerus, which formerly included the natural ball of the anatomic shoulder.
The socket also features a metal peg that allows the patient’s native bone to grow into the implant. The Comprehensive Reverse Shoulder, which these surgeons also designed, is entirely cementless. Both sides of the joint feature the ability for native bone to grow into, and become integrated with the implant.
Complications
Complications are rare in total shoulder replacement, but can include:
An arthritic shoulder is often very tight to begin with. However, if post-operative stiffness is a problem in a shoulder in which motion was restored during surgery, the stiffness is usually a result of incomplete rehabilitation. Continued rehabilitative efforts are usually effective in restoring shoulder motion and strength.
Shoulder replacement surgery recovery and rehabilitation
After leaving the operating room with the arm immobilized at the side in a removable canvass arm sling, the patient will wake up in the recovery room. “Normally,” , “patients will wake up from surgery with pain due to surgery, but not the same type of pain they have experienced due to their arthritis. Arthritic pain is largely absent from that point forward.”
The day after surgery
X-rays will be taken to document that the implant is properly positioned. Then, if the range of motion and stability of the implant are confirmed, physical therapy will begin that same day. The shoulder will be immobilized by a sling during the early rehabilitation phase to permit the tendons which have been repaired to heal. This sling is removable for showering and for rehabilitation exercises. “As patients begin the physical therapy program, they notice that shoulder mobility is easier,”, “and the hard grating and grinding so typical of an arthritic shoulder is no longer there.”
Recovery time
It generally takes eight weeks or more for patients to recover. It may be several months before a patient may do heavy labor or strenuous strength exercises. The usual timelines for recovery are as follows: